Additional Information
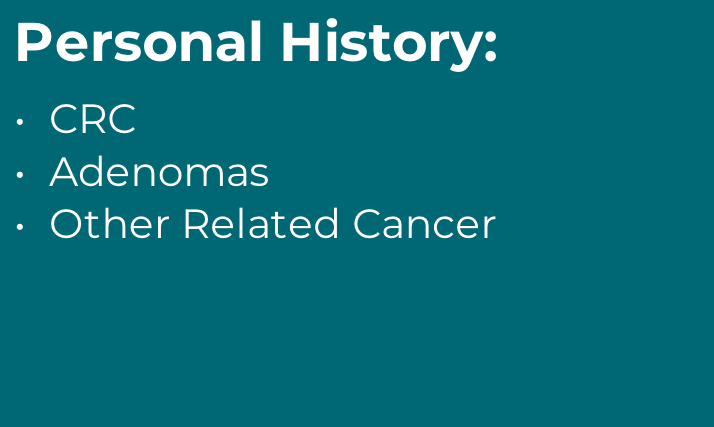
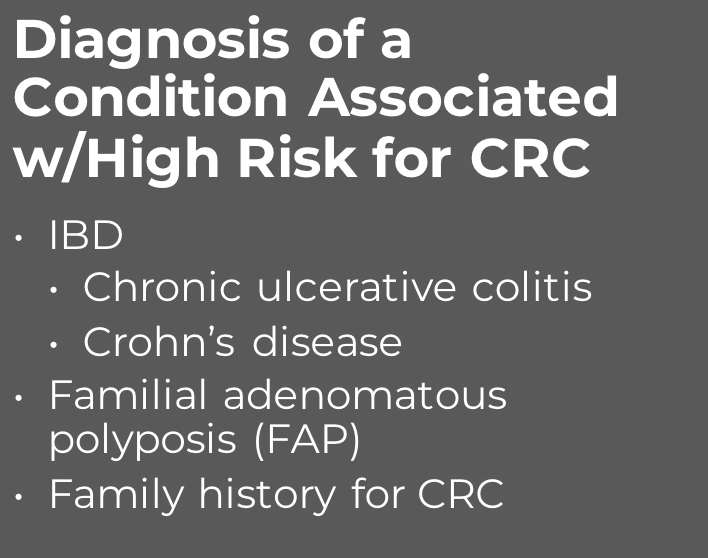
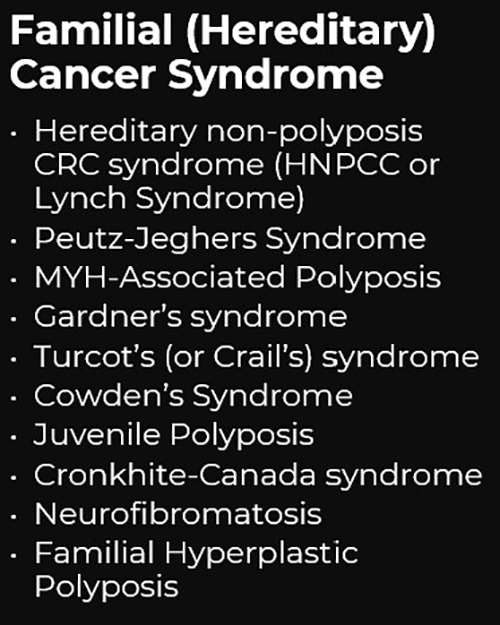
The multi-target stool DNA (mt-sDNA) is intended for the qualitative detection of colorectal neoplasia associated DNA markers and for the presence of occult hemoglobin in human stool.1 A positive result may indicate the presence of colorectal cancer (CRC) or advanced adenoma (AA) and should be followed by colonoscopy.1 mt-sDNA is indicated to screen adults of either sex, 45 years or older, who are at typical average-risk for CRC.1 mt-sDNA is not a replacement for diagnostic colonoscopy or surveillance colonoscopy in high risk individuals.1