An Evaluation of a Multi-target Stool DNA (mt-sDNA) Test, Cologuard®, for CRC Screening in Individuals Aged 45-49 and at Average Risk for Development of Colorectal Cancer (Act Now Study). This study was a prospective, cross-sectional, multicenter study of individuals aged 45-49 years at average risk for colorectal cancer (CRC).1 The primary outcome measure was to determine the specificity of the mt-sDNA test for advanced colorectal neoplasia using colonoscopy as the reference standard. A total of 983 participants were enrolled from 31 sites across the US from November 2018 to June 2019. The mt-sDNA test demonstrated high specificity (95.2%) in this population.1
ACT NOW STUDY DESIGN1,a

Participant Disposition1
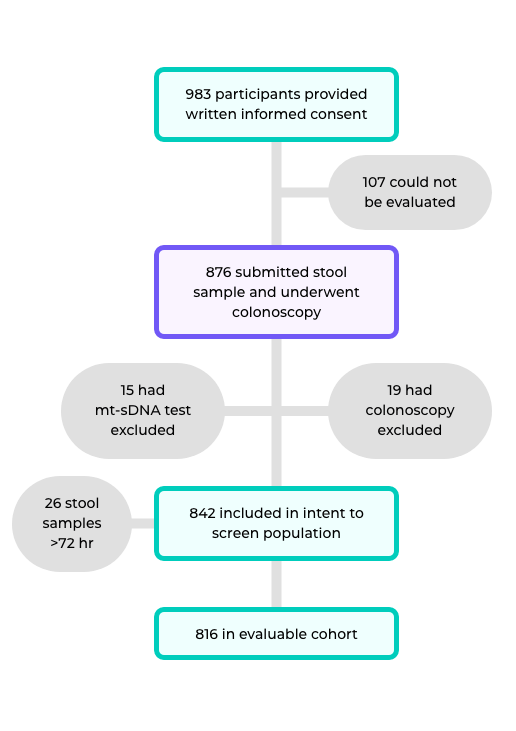
- The evaluable cohort included 816 individuals, and the mean age was 47.8 years and included 47.7% women1
- 84% of the enrolled participants were white1
- Participants in the enrolled, intent-to-screen, and evaluable cohorts were similar in age, sex, and race/ethnicity1
mt-sDNA DEMONSTRATES HIGH SPECIFICITY IN INDIVIDUALS AGED 45-49 YEARS1
|
|||||
| Total | CRC | APL |
Non-advanced Neoplasia |
Negative Findings |
|
| n (%)c | 816 | 0 (0.0%) | 49 (6.0%) | 253 (31.0%) | 514 (63.0%) |
| mt-sDNA Positive | 53 | 0 | 16 | 18 | 19 |
| Most Advanced Finding | Colonoscopy (n=816) | mt-sDNA (n = 816)d | |
| n | Positive Results, n |
Specificity, %
(95% CI) |
|
|
All non-advanced, non-neoplastice findings, and negative results on colonoscopy |
767 | 37 | 95.2 (93.4-96.6) |
| Negative results on colonoscopy | 514 | 19 | 96.3 (94.3-97.8) |
- Specificity did not differ by sex (94.9% male vs 95.4% female; P=0.75) or race (94.5% white vs. 98.9% Black or African-American; P=0.36 across all races)1
- The specificity is higher (less false positives) in the 45–49-year-old population1 than in those 50 years and older in the DEEP-C study (87%)2
- The higher specificity in this younger age group is in line with the expected lower prevalence of any colorectal neoplasia, lesions that cause bleeding, and lower background methylation in stool samples3
- Limitations of the study include possible selection bias, most participants were White individuals, and CRC screening adherence in this cohort is not well defined1
- The incidence and mortality of CRC in adults <50 years is increasing, making it more critical to detect CRC and precancerous lesions at early stages4
APL: high-grade dysplasia/cancer in situ, any size; villous growth pattern (≥25%) of any size; adenomas ≥10 mm, and serrated lesions ≥10 mm.
References
1 Imperiale TF, Kisiel JB, Itzkowitz SH, et al. Specificity of the multi-target stool DNA test for colorectal cancer screening in average-risk 45-49 year-olds: A cross-sectional study. Cancer Prev Res. 2021;14(4):489-496.
2 Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014;370(14):1287-1297.
3 Ahlquist DA. Multi-target stool DNA test: a new high bar for noninvasive screening. Dig Dis Sci. 2015;60:623-633.
4 Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68(4):250-281.
Footnotes
a Standard deviation=19.4 days.
b Findings identified during colonoscopy.
c Also indicated as prevalence, used in positive predictive (PPV) and negative predictive (NPV) values.
d The evaluable cohort included only participants with a usable mt-sDNA and complete colonoscopy. Participants with stool samples received outside of the 72-hour mt-sDNA processing window, incomplete/not reportable colonoscopies, and other major protocol violations (inclusion/exclusion criteria not met) were excluded.
e Non-neoplastic findings=hyperplastic polyps, lymphoid aggregates, others.
Last updated: 04/22/2023